Healthcare Fraud Analytics Market Dynamics
Driver: Increased number of patients seeking health insurance
Over the years, the number of people benefitting from various healthcare schemes has grown considerably. A couple of reasons contributing to the growth of the health insurance market include the rise in the aging population, growth in healthcare expenditure, and increased burden of diseases. In the US, the number of citizens without health insurance has significantly decreased, from 48 million in 2010 to 28.6 million in 2016. In 2017, 12.2 million people signed up for or renewed their health insurance during the 2017 open enrollment period (Source: National Center for Health Statistics).
Emerging markets such as Asia promise significant growth in health insurance coverage, mainly due to increasing government initiatives, rising government and private investments for promoting medical insurance, and growing income levels. This growth is aided by the increasing affordability of health insurance for the middle class in this region and the rising awareness regarding the benefits of health insurance. In the UAE, as per a new regulatory policy (2017), any citizen residing and working in the UAE needs to be insured medically. Such regulatory changes in the buying behavior of employers (from employer-based plans to providing individual spending allowances to the staff) are driving the health insurance market in the region.
Restraint: Limitations in the data capturing process in Medicaid services
As per the US Department of Health and Human Services findings of 2018, national Medicaid data has shortcomings that could hinder the process of fraud detection in the public sector. The OIG claims that Medicaid data is often incomplete and inaccurate; this affects the process of detecting fraudulent claims and results in the wastage of billions of dollars due to FWA.
Opportunity: Emergence of social media and its impact on the healthcare industry
The healthcare industry is changing at an incredible rate, and one of the major contributors to this change is the increasing popularity of healthcare communication through social media.
Download PDF Brochure @ https://www.marketsandmarkets.com/pdfdownloadNew.asp?id=221837663
This vast network of healthcare influencers, leaders, patients, providers, organizations, and governmental entities creates a massive amount of healthcare data on a regular basis. This data, if segregated, segmented, and analyzed in a meaningful way, can offer incredible value for improving treatment efficiencies and health outcomes. This has created a demand for data aggregation and analytical tools and thus acts as an opportunity for the healthcare fraud analytics market during the forecast period.
Challenge: Time-consuming deployment and the need for frequent upgrades
The deployment of fraud analytics solutions is a time-consuming process. The process involves creating user interfaces, new databases, and predictive models; evaluating and deploying models, and monitoring their effectiveness. In this process, data analysts continuously run algorithms until they get the most effective predictive model.
At times, analysts may not find the appropriate predictive model for expected outcomes, which results in time wastage. This means they must start the same process again with new data. Thus, if data analysts fail at one stage, the whole process is disturbed. Furthermore, the software requires frequent upgrades, as fraudsters constantly change tactics. This adds to the total cost of fraud analytics solutions.
[176 Pages Report] Fraud analytics is the efficient use of data analytics and related business insights developed through statistical, quantitative, predictive, comparative, cognitive, and other emerging applied analytical models for detecting and preventing healthcare fraud.
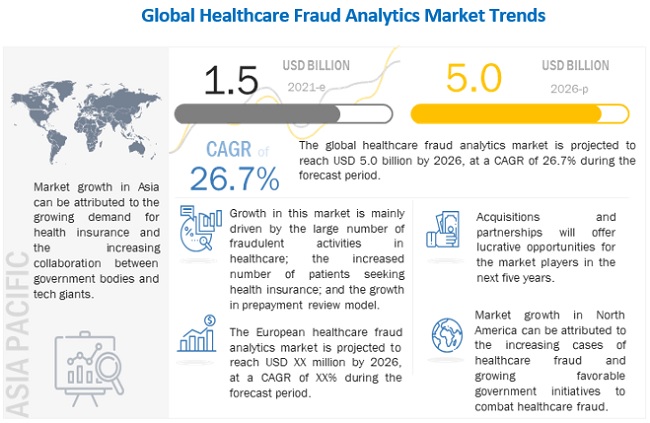
The global healthcare fraud analytics market is projected to reach USD 5.0 billion by 2026, at a CAGR of 26.7% during the forecast period. Market growth can be attributed to a large number of fraudulent activities in healthcare, increasing number of patients seeking health insurance, high returns on investment, and the rising number of pharmacy claims-related frauds. However, the dearth of skilled personnel is expected to restrain the growth of this market.